FINAL PRACTICAL EXAM SHORT CASE- 47 YEAR OLD FEMALE WITH FEVER AND JOINT PAINS
General Medicine final practical exam- Short case
Reg no: 1701006068
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION
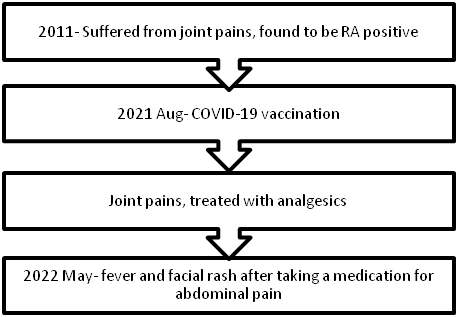
TIMELINE OF EVENTS:
A 47-year-old male has presented to the hospital on 02 June 2022 with the chief complaints of
- fever
- rash over the face
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic ten years ago then she developed joint pains in both knees and ankles, then both hands. There was swelling, and stiffness in the morning for around 15 minutes, with movement restrictions. The patient was treated at a private hospital and was diagnosed as RA POSITIVE and was prescribed diclofenac.
- Patient had a history of vision deterioration and began wearing spectacles at the age of 15 years, but the loss of eyesight was gradual, progressive, and painless, and he was declared legally blind. No relevant drug or trauma history .
- not a known case of hypertension , diabetes, asthma, epilepsy, TB.
- married
- normal appetite
- takes mixed diet
- bowel movements: regular
- micturition is normal
- no known allergies
- addictions: none
Done after obtaining consent. The patient is conscious, incoherent, cooperative, well-nourished, and well -oriented to time, but not oriented to place and person.
Pallor: present
- No icterus, cyanosis, clubbing,lymphadenopathy, edema.
VITALS
- Temperature - afebrile
PULSE:86BPM
- BP:120/80mm hg
- RR:16cpm
inspection: shape of the chest is normal
no visible neck veins
No rise in JVP
palpation: all inspectory findings are confirmed
apex beat normal at 5th ics medial to mcl
no additional palpable pulsations or murmurs
percussion: showed normal heart borders
auscultation: S1 S2 heard no murmurs or additional sounds
2. Respiratory system:
inspection: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
palpation: Insp findings are confirmed
percussion: normal resonant note present bilaterally
auscultation: normal vesicular breath sounds heard
3. GIT:palpation - inspectory findings are confirmed
no organomegaly, non tender and soft
percussion- normal resonant note present, liver border normal
auscultation-normal abdominal sounds heard, no bruit present
4. CNS:
Higher mental functions
- conscious and cooperative coherent
- oriented to time, place and person.
- memory- recent and immediate memory intact
CRANIAL NERVE EXAMINATION
2nd cranial nerve. Right. Left
Visual acuity. Counting fingers
Counting fingers postive
Direct light reflex present. Present
Indirect light reflex present. Present
Perception of light. Present. Present
Remaining cranial nerves normal.
SENSORY :
touch, pressure, vibration, and proprioception are normal in all limbs
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
CBP
- Hemoglobin- 6 gm/dl
- PCV- 21 %
- TLC- 8200/ cumm
- RBC- 2.5 million/cumm
- Platelets- 1.32 lakhs/ml
1.INJ PIPTAZ 4.5 gm IV/ TID.
2.INJ METROGEL100 ML IV/TID
3.INJ NEOMOL1GM/IV/SOS
4.TAB CHYMORAL FORATE PO/TID
5.TAB PAN 40 MG PO/ OD.
6.TAB TECZINE10 MG PO/OD
7.TAB OROFERPO/OD.
8.TAB HIFENAC-P PO/OD
9HYDROCOTISONE cream 1%on face for 1week.






Comments
Post a Comment