85 YEAR OLD MALE WITH CVA
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name: Sreshta J
Roll no: 48
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION
An 85-year-old male has presented to the casualty on 23 September 2021 with the chief complaints of
- Weakness of left upper and lower limbs since 15 days
- Shortness of breath (SOB hereafter) since 15 days
- Dysphagia since 10 days
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 15 days ago then he developed weakness of the left upper and lower limbs. He went to a local doctor who treated him symptomatically. He was asked to return for a follow up 3 days ago and the doctor advised him to admit to the hospital. The attendants brought him to our tertiary care hospital instead for free treatment.
He also complained of giddiness
WEAKNESS:
- It was sudden in onset.
- he couldn't lift his left upper limb at all
- no h/o trauma or seizures.
- he has grade 5 SOB
- since 2 days
- relieved on sitting upright
- no similar complaints in the past.
- not a known case of diabetes, asthma, epilepsy, TB.
- diagnosed with hypertension 7 months ago and has been using medication since
- married
- normal appetite
- takes mixed diet
- bowel movements: loose stools
- micturition is normal
- no known allergies
- addictions: none
Done after obtaining consent, in a well-lit room, in the presence of an attendant, with adequate exposure. The patient is conscious, coherent, cooperative, well-nourished, well -oriented to time, place, person.
- No pallor icterus, Cyanosis, Koilonychia, Generalised Lymphadenopathy, Pedal oedema and clubbing
- Gynaecomastia is seen
- Muscle wasting is observed
VITALS at the time of admission:
- Temperature - afebrile
- Pulse rate- 100 bpm
- BP- 140/90 mm Hg
- Respiratory rate- 22/min
- Height- 170cm
- Weight- 38kg
2. Respiratory system: COPD?
- SOB- grade 4
4. CNS:
- facial asymmetry is seen
- the mouth and tongue have deviated to the right side
Videos: 1. Exaggerated biceps reflex
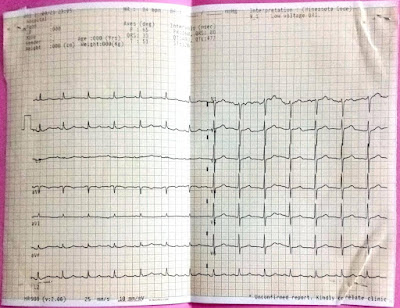
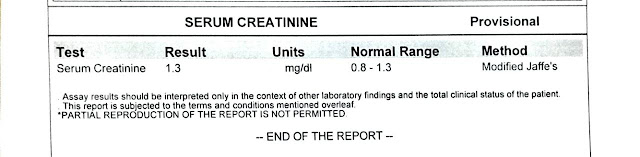
INVESTIGATIONS:
CBP
CXR










Comments
Post a Comment