50 YEAR OLD MALE WITH TUBERCULOSIS AND RETROVIRAL DISEASE
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name: Sreshta J
Roll no: 48
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION
A 50-year-old male has presented to the casualty on 15 September 2021 with the chief complaints of
- fever and diarrhoea for 1 month
- cough since 10 days
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 30 days ago when he developed a fever
FEVER:
- It was an intermittent and low-grade fever associated with chills and rigours.
- no other associated symptoms like nausea, vomiting and headache.
- multiple episodes per day following food intake
- watery in consistency
- greenish yellow color
- not associated with abdominal pain
- cough with sputum since 10 days
- more in the nights
- not a known case of hypertension, diabetes, asthma, epilepsy.
- suffered from TB 20 years ago, used medication for 9 months.
- married
- lost appetite
- takes mixed diet
- bowel movements: loose stools
- micturition is normal
- no known allergies
- addictions: has been addicted to playing cards since 15 years
Done after obtaining consent, in a well-lit room, in the presence of an attendant, with adequate exposure. The patient is conscious, coherent, cooperative, well-nourished, well -oriented to time, place, person.
- No icterus, Cyanosis, Koilonychia, Generalised Lymphadenopathy, Pedal oedema and clubbing
- pallor is seen
VITALS at the time of admission:
- Temperature - afebrile
- Pulse rate- 110 bpm
- BP- 70/60 mm Hg
- Respiratory rate- 40/min
- Height- 170cm
- Weight- 38kg
2. Respiratory system:
- Crepitations in the right infraclavicular region
4. CNS: No focal deficit
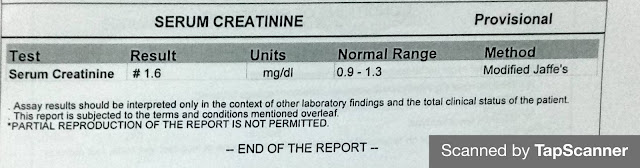
INVESTIGATIONS:
HBsAg- rapid- negative
Anti HCV Antibodies- non-reactive
CBP
ECG
LFT
HBsAg- rapid- negative
Anti HCV Antibodies- non-reactive
Chest X-ray
Serum Electrolytes
TREATMENT PLAN (given on 15 September 2021):
- IVF - NS 75ml/hr
- Inj metrogyl 100ml iv tid
- pantop 40mg iv od
- tab ciprofloxacin 400mg po bd
- vitals monitoring
17 September 2021
VOMITINGS:
- 5 episodes during night
- watery in consistency
- greenish yellow in color
18 September 2021
VOMITINGS:
- 1 episode following food intake
- contents: food










Comments
Post a Comment