25 YEAR OLD MALE WITH VIRAL PNEUMONIA AND KARTAGENER SYNDROME
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name: Sreshta J
Roll no: 48
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
I have further referred the case from my Senior’s elog. Thank you for the consent sir.
https://katanaveenkumar.blogspot.com/2021/08/25-yr-old-male-with-shortness-of-breath.html
Following is the view of my case :
CASE PRESENTATION
A 25-year-old male has presented to the OPD on 25 August 2021 with the chief complaints of
- shortness of breath since 10 days
- pedal oedema since 10 days
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 10 days ago when he developed shortness of breath (SOB from hereafter) after consuming 90ml of whisky. He first consulted an RMP, who gave him fluids and was later referred to our tertiary care hospital.
He was diagnosed with dextrocardia on 4th day of delivery.
SOB:
- He has been suffering from SOB since his teens. As the patient recalls his first episode happened when he was 14 years old while he was playing in school. Copious amounts of expectoration were seen. It was yellowish in colour and non-foul smelling.
- Has a history of respiratory tract infections which occur almost twice a year. It is aggravated by exposure to cold temperature and relieved by taking medication.
- Was in a bike accident 14 days ago and sustained a head injury.
- Refused to go to the hospital to get checked
- Developed oedema 3 days later which extended up to the knee.
PAST HISTORY :
- not a known case of hypertension, diabetes, asthma, epilepsy or tuberculosis.
- married
- lost appetite
- takes mixed diet
- bowel movements are regular
- micturition is normal
- no known allergies
- addictions: has been consuming alcohol twice weekly for 5 years.
Done after obtaining consent, in a well-lit room, in the presence of an attendant, with adequate exposure. The patient is conscious, coherent, cooperative, well-nourished, well -oriented to time, place, person.
- No pallor, icterus, Cyanosis, Koilonychia, Generalised Lymphadenopathy
- Pedal oedema and clubbing of the fingernails was seen.
 |
| Fig: Clubbing of fingernails |
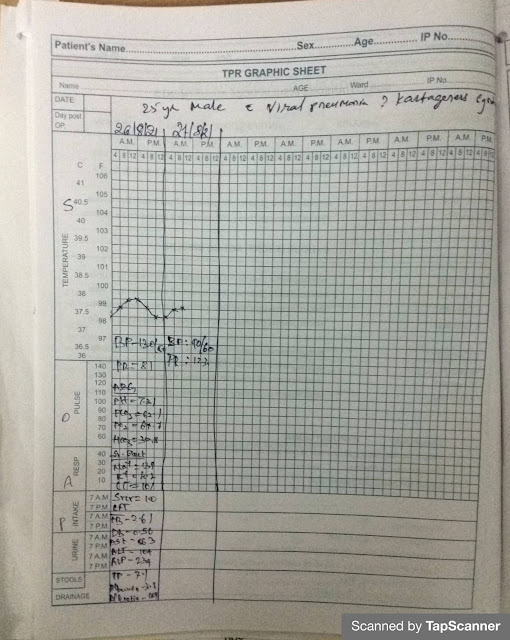
VITALS at the time of admission:
- Temperature - 97.6 degrees Fahrenheit
- Pulse rate- 120 bpm
- BP- 150/70 mm Hg
- Respiratory rate- 40/min
- SpO2- 41% at room temperature
2. Respiratory system:
- Dyspnoea - present
4. CNS: No focal deficit
INVESTIGATIONS:
CBP
- Hb- 17.8gm/dl
- total count- 12600 cells per cumm
- neutrophils- 82%
- leucocytes- 12%
- PCV- 55.6vol%
- RBC- 6.3million/cumm
- Platelets- 1.3lakhs/cumm
- Impression: Normocytic normochromic blood picture with neutrophilic leucocytosis and mild thrombocytopenia.
ECG
ABG
LFT
Serology- negative for Covid-19
Chest X-ray (PA View)- Dextrocardia
USG Abdomen
Serum Electrolytes
RBS- 101mg/dl
Serum Creatinine- 1mg/dl
Serum urea- 48mg/dl
PROVISIONAL DIAGNOSIS:
?Kartagener syndrome- Dextrocardia, situs inversus & bronchiectasis
?Viral pneumonia
TREATMENT PLAN (given on 25 August 2021):
- Head end elevation
- O2 inhalation to maintain SpO2 at 92%
- Nebulizer with Duolin 8th hourly
- BP, PR, SpO2, temperature monitoring 4th hourly
- Inj Lasix 40 mg BD
- Inj Thiamine 1 ampoule in 100ml NS IV BD
- Inj Levofloxacin 750mg IV OD
- Inj Doxycycline 100mg IV BD
- Inj Ceftriaxone 1gm IV BD
SOAP NOTES:
26 August 2021
Subjective: Shortness of breath
Objective:
- Temperature - afebrile
- Pulse rate- 133bpm
- Respiratory rate- 45/min
- SpO2- 95% on 15 lit of O2
- CVS: S1 & S2 heard
- Respiratory system: Dyspnoea - present
- Abdomen: Soft and non-tender
- CNS: No focal deficit
- no RWMA
- mild PAH
- good LV systolic function
- IVC dilated
- Kartagener syndrome
- Viral pneumonia
- Inj Levofloxacin 750mg IV OD
- Inj Doxycycline 100mg IV BD
- Inj Ceftriaxone 1gm IV BD
- Inj Lasix 20mg IV BD only if systolic blood pressure > 110mmHg
- Nebulizer with Duolin 8th hourly
- Inj Thiamine 1 ampoule in 100ml NS IV BD
- BP, PR, SpO2, temperature monitoring 2nd hourly
- Intermittent CPAP every 2nd hourly
- Temperature charting
- Temperature-98 F
Bp-110/70 mmHg
- PR- 80bpm
- RR -17cpm
- CVS-S1, S2 heard
- RS- BAE+
- spo2-98%on 7 lit of oxygen
Assessment:
- Viral Pneumonia
- Kartergener syndrome
1. Inj.Levofloxacin 750mg/iv/BD
2. Inj Doxycycline 100mg/IV/BD
3. Inj.Ceftriaxone 1gm/iv/BD
4. Inj.Lasix 20mg/Iv/BD
5. Inj.Thiamine 1amp in 100ml NS Iv/BD
6. Nebulisation with Budecort 12th hourly
7. Temperature charting
8. Bp/PR/RR/spo2 monitoring
9. Intermittent CPAP every 2nd hourly
- Temperature-98 F
- Bp-100/70 mmHg
- PR- 88bpm
- RR -18cpm
- CVS-S1, S2 heard
- RS- BAE+
- spo2-98%on 7 lit of oxygen
Assessment:
- Viral Pneumonia
- Kartergener syndrome
Plan of care:
1. Inj.Levofloxacin 750mg/iv/BD
2. Inj Doxycycline 100mg/IV/BD
3. Inj.Ceftriaxone 1gm/iv/BD
4. Inj.Lasix 20mg/Iv/BD
5. Inj.Thiamine 1amp in 100ml NS Iv/BD
6. Nebulisation with Budecort 12th hourly
7. temperature charting
8. Bp/PR/RR/spo2 monitoring
9. Intermittent CPAP every 2nd hourly
31 August 2021
- Temperature-98 F
- Bp-120/70 mmHg
- PR- 88bpm
- RR -18cpm
- CVS-S1, S2heard
- RS- BAE+
- spo2-96%on 5 lit of oxygen
- spo2-74%without oxy mask
Assessment:
- Viral Pneumonia
- Kartergener syndrome
- HRCT report
Plan of care:
1. Tab.Levofloxacin 750mg/iv/BD
2. TabDoxy 100mg/IV/BD
3. Inj.Ceftriaxone 1gm/iv/BD
4. Inj.Thiamine 1amp in 100ml NS Iv/BD
5. Nebulisation with Budecort 12th hourly
7. Bp/PR/RR/spo2 monitoring
8. Intermittent CPAP every 2nd hourly
6. temperature charting
- Temperature- afebrile
- Bp-110/70 mmHg
- PR- 84bpm
- RR -14cpm
- CVS-S1, S2heard
- RS- Crepitus heard
- spo2-84% at RT
Assessment:
- Viral Pneumonia
- Kartergener syndrome
- Inj.Thiamine 1amp in 100ml NS Iv/BD
- Nebulisation with Budecort 12th hourly
- O2 inhalation to maintain SpO2 at 94%
- Bp/PR/RR/spo2 monitoring









Comments
Post a Comment